Healing Feet, Avoiding Amputation

GitHub page
Ensure or Establish Adequate Arterial Inflow
With revascularization, 1-year limb salvage rates among patients with peripheral artery disease (PAD) and a foot ulcer, foot infection, or foot gangrene with is 90% (see review).
If PAD is untreated or unrecognized, 1-year limb salvage rates are 50-60% (see review).
Thus, the identification and treatment of PAD in patients with foot ulcers may be the single most influential factor in amputation prevention. Revascularization is cost-effective and may even provide cost-savings in frail, elderly patients.
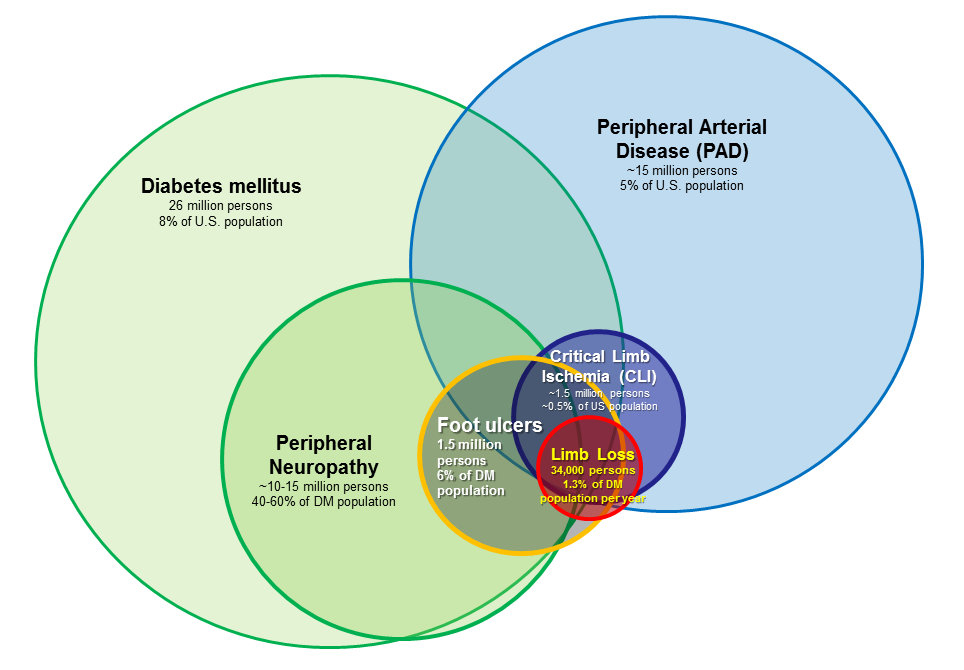
(Venn diagram from our 2013 “System of Care” review paper)
A formal decision analysis identified these as the two most sensitive strategies to identify PAD in patients with foot ulcers:
strategy 1: non-invasive testing (esp. toe-brachial index or skin perfusion pressure) for everyone, angiogram to investigate abnormal results = 83% sensitivity.
strategy 2: pedal pulse exam first; non-invasive testing (esp. toe-brachial index or skin perfusion pressure) to corroborate adequate arterial perfusion vs. angiogram to investigate abnormal pulse exam findings = 92% sensitivity.
Reserving non-invasive testing for patients with weak or absent pedal pulses, then doing angiography only if this is abnormal is associated with a low sensitivity rate in finding PAD.
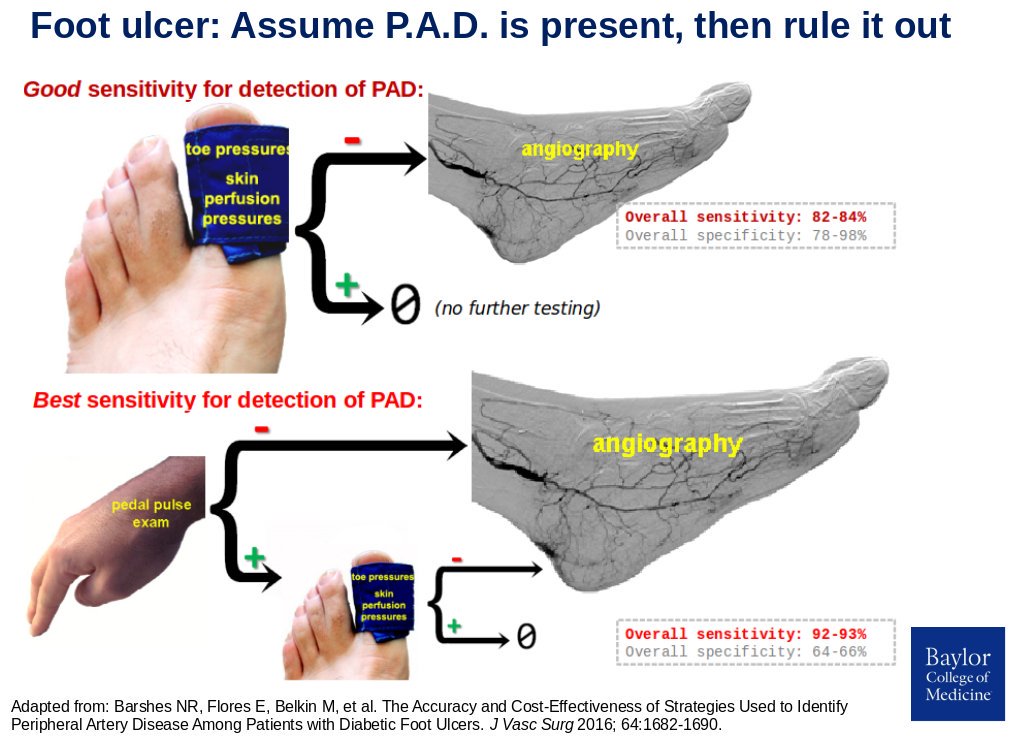
Simply put, these findings suggest that all patients with foot ulcers should get objective testing, either in the form of an angiogram or non-invasive testing.
.
| In addition, consider angiography if any of the following specific situations are present: |
|---|
| pedal pulses weak or absent |
| continuous wave Doppler signal is monophasic |
| toe-brachial index <0.7 |
| toe pressure <60mmHg |
| lowest ABI (lower ankle pressure:highest brachial pressure) <0.9 |
| ulcer size >3cm |
| infection requiring >3cm incision for drainage |
| ulcers in multiple locations/angiosomes |
| foot ulcer in area supplied by single angiosome: heel, dorsal foot |
| anticipated Lisfranc amputation, rotational flap, or free flap reconstruction |
For some further explanation, consider these brief videos on bedside evaluation and non-invasive lower extremity arterial testing for PAD. For further detail still, read this chapter on non-invasive testing for peripheral artery disease.
Our hospital’s vascular surgery experience began as part of the Baylor College of Medicine peripheral vascular surgery training program initiated by Dr. Michael E. DeBakey in the 1980s (K. Mattox, The History of Surgery in Houston). We currently have the highest-volume VA vascular surgery service in the country. Together with other rotations, our program’s experience in limb salvage have put our surgical trainees at the 86th percentile for peripheral obstructive cases. These are some selected details to help you be involved in cases at our hospital.
Infrainguinal Endovascular Procedures
In the clinic, consider: (1) indication; (2) feeling for bilateral femoral pulses, ipsilateral popliteal and pedal pulses; and (3) bedside vein mapping. Consult our vascular medicine colleagues for long-term optimization of medical management (patient does NOT need to be seen prior to surgery). If eGFR<30mL/min, enter delayed orders for pre-admission that will include normal saline at 0.5mL/kg/hr, vitamin C 500mg BID, acetylcysteine 600mg PO BID.
In planning the case, consider: (1) indication/wound location & relevant angiosome(s); (2) antiplatelets/anticoagulants; (3) baseline eGFR; (4) pulse exam & vein mapping (from clinic note); (5) any previous imaging; and (6) any clinical that needs management prior to the angiogram (incl. orthopnea, contrast allergy). Posting should generally use the 36247 code, NOT any procedural code beginning with a 7.
Basic steps of my preferred approach: Bentson to get 5Fr sheath in; Contra/Omni to the aorta. Up-and-over with floppy angled Glidewire. Try to get floppy Glidewire to popliteal. If successful, place a 135cm Quickcross catether for the angiograms starting in distal leg. Visualize more proximal segments later. See here for preferences of other staff surgeons.
Ultimately, these seven digital subtraction angiography runs with the following power injector settings for the affected extremity:
- popliteal at 20° oblique, 5x5
- upper calf w tibia-fibula separated, 5x5-10
- calf w tibia-fibula separated, 5x5-10
- craniocaudal foot shot magnifiedx1, 4x12
- lateral foot shot magnified x1, 4x12 Then, after withdrawing the catheter more proximally:
- AP thigh, 5x5
- femoral at 15° oblique, 5mL/sec for 5mL.
If severely impaired eGFR, consider carbon dioxide angiography with this setup.
If intervention: long Amplatz wire through Quickcross + 45cm 6Fr (if SFA/pop) or 55/70cm 5Fr (if tibial). Cross (0.014” or 0.018” system for tibials, 0.035” system for SFA), confirm location with DSA, PTA, consider stent.
After the case: bedrest for six hours. Generally an outpatient procedure. Inpatient observation again only if needed for hydration, renal protection. Discharge without outpatient narcotics (Tylenol only), Plavix bolus if intervention. Discuss cilostazol otherwise.
Procedural Details for Infrainguinal Bypasses
In the clinic before the operation, consider: prior operations in index extremity; angiogram results; vein mapping (NOT done in vascular lab) if not already done during previous hospital stay. Pre-admitted is discouraged, regardless of eGFR/creatinine. Use the CHADS-Vasc2 score to determine need for a “bridge” for patients on anticoagulants for atrial fibrillation.
Before the case, consider: (1) indication; (2) hemoglobin; (3) eGFR; (4) planned conduit (single-segment saphenous vein, then spliced arm vein, then PTFE with distal vein patch), (5) baseline anti platelet / anticoagulation medications. I will mark vein course using ultrasound BEFORE the patient gets to the room.
On the field: 4-0 silk ties; 7-0 Prolene. magnet pad, Ioban x3. Supine, left arm tucked (unless left arm vein harvest is planned). Drape just above the umbilicus. Isolation bag if tibial/pedal target, stockinette otherwise. If foot wound: foot should be prepared with chlorhexidine scrub in preference to not iodine-based solutions. Our OR team generally knows to open 4-0 silk ties, 7-0 Prolene, vein solution and other typical accoutrements; therefore, no list is included here. All members of the team should do a full five-minute hand scrub.
Five main steps: 1) vein harvest; 2&3) distal & proximal exposures; 4) tunneling + anastomoses; 5) closure. Read this leg bypass chapter for more details relevant to both femoropopliteal and femorotibial bypass.
The bundle we’ve employed to reduce surgical site infections by 67%:
- Minimize hospital pre-admission.
- Methicillin-resistant Staphylococcus aureus decontamination protocol with mupirocin nasal ointment, chlorhexidine wipes or shower. This is routinely done through our outpatient clinic.
- Vancomycin in wound ONLY if re-do case AND no vein in the field.
- Interrupted 2-0 Vicryl to close dead space.
- Subcuticular skin closure with 4-0 Monocryl. Avoid staples in groin incisions.
- Negative pressure wound therapy (transparent dressing “window panes”, Adaptec, black sponge, more transparent dressings).
Post-operative Orders following Infrainguinal Bypass
Immediate post-op: .
Admit = 5E or 5B (not 5A unless specific criteria are met).
Diagnosis = s/p ___, Condition = ___.
Vitals qshift; do NOT request strict Is &Os.
Notify physician for SBP>160mmHg or <90mmHg, diastolic>100mmHg, pulse <55 or >110/min, urine = N/A.
Activity order: "Weight bearing on affected foot only with offloading shoe or boot".
Nursing text order: "Please do not manipulate leg wrap. Do not move or adjust wrap to find Doppler signals that do not already have windows for monitoring." (for patients with leg wrap)
Nursing text order: "Incisional wound VAC to -75 mmHg continuous suction, low intensity."
(if present in groin wound) Nursing text order: "Keep overhead lights on and curtains open during daytime hours (7A-9PM)".
Nursing text order: "Up to chair with assistance for at least three hours daily. Thank you."
Diet: Carbohydrate controlled if diabetes; volume restricted if CKD5/ESRD. IV fluids: NS @ ~0.5mL/kg/hr x12 hours.
The "SAAVE THe LIMB" medication bundle foot ulcer or gangrene patients:
S = Statin medication.
A= Aspirin 81mg Antibiotic:systemic (perioperative x24h + isolate-directed) ± topical (cadexomer iodine).
V= Vitamin C 500mg PO BID and, if diabetes diagnosis, Vitamin D3 25mg PO daily also.
E= ”Ensure” BID (use Glucerna SR, however, as it has lower added sugar).
T= Tylenol PRN for pain or temperature >100.4°F (38°C)
He= Heparin subcutaneous q8h (or Lovenox) and Home medications.
L= Lactobacillus 2 capsules PO BID.
I= Insulin: 50% of long-acting insulin home dose + medium-dose sliding scale until on solid food diet, then resume home regimen.
18. M= Multivitamin 1 cap daily.
19. B= Blood pressure meds, baseline + at least one PRN for SBP>140mmHg.
Other orders:
22. Labs upon arrival: blood count, basic metabolic panel and PT/PTT/INR. (In active orders, not delayed order set.)
23. Labs for AM POD#1: hemoglobin and basic metabolic panel in morning. Add baseline brain naturetic peptide (BNP) if known CHF.
SCHEDULED components of the multimodal analgesia bundle (adapted from the UT Houston trauma group):
1. Acetaminophen 500 milligrams PO q6h (scheduled).
2. Gabapentin 300mg (--> up to 1200mg if already on home dose) PO q8hr thereafter. If eGFR <30mL/min, 200 mg PO once daily (--> max dose 700 mg once daily).
3. Lidocaine 5% topical patches (up to three) x12 hours on adjacent and proximal to surgical site, then 12 hours off.
4. Docusate 100 mg / sennosides 8.6mg (combination pill) PO every 12 hours.
AS NEEDED components of the multimodal analgesia bundle:
5. Tramadol 50 or 100 mg PO q6h PRN mild pain. For eGFR <30 mL/min, 50 mg PO every 6 hours. Contraindications: history of seizures, monoamine oxidase inhibitor (MAOI) use, or selective serotonin reuptake inhibitor (SSRI) use.
6. Codeine 30mg tablet (i.e. without acetaminophen) q6h PRN moderate pain.
7. Morphine 4mg IV q3 hours PRN severe pain.
8. Bisacodyl suppository 10 mg rectally daily PRN for no bowel movement.
9. Polyethylene glycol 3350 17 g PO every 12 hours.
Options if still not controlled: morphine 15-30mg PO q4h or fentanyl patch. Do NOT use non-steroidal anti-inflammatory (NSAID) medications because of the high incidence of chronic kidney disease and acute kidney injury among our inpatients.
Links for evidence supporting aspects of this order set include systematic review of multiple large randomized trials showing that Lactobacillus reduces Clostridium difficile-associated diarrhea{1,2,3}; a randomized trial showing vitamin C supplementation significantly improves foot ulcer healing{4}; and randomized trials showing vitamin D supplementation has significant benefits for diabetic foot ulcer healing{5} and glycemic control{6}.
MINIMIZE or AVOID oxycodone (Percocet), hydromorphone (Dilaudid), benzodiazepines, and muscle relaxants.
Post-Operative Day #1: Main goals are generally out of bed. Discuss patient with staff surgeon by 745am.
Additional orders, post-operative day #1:
1. Out of bed to chair during day, with first transfer by noon.
2. Foley out, wean any supplemental O2.
3. Saline (not herparin) lock IV.
4. Consider furosemide if edema present.
5. Order Iodosorb (if foot infection present) or collagenase (if uninfected foot ulcer) to bedside for dressing change on post-operative day #2.
6. Resume home insulin regimen.,br> 7. PT consult in transfer orders.
8. Do NOT order AM labs for POD #2.
Post-Operative Day #2: Ensure out or bed. Remove and replace leg wrap (ok to give patient break for a few hours) and foot dressing, conforming to contemporary strategies for wound healing. Tell patient to make plans to get home day 4 or work with case manager, social worker, and nurse practicioner to identify other discharge plans.
Additional orders, post-operative day #2:
1. Order POD #3 AM hemoglobin +/- repeat BNP. BMP only if ESRD, prior electrolyte abnormalities, or other clinical indication.
2. Change acetaminophen order from scheduled to PRN q6h. 3. Prosthetics consult for DH walker (if patient does not already have one). Look under "Footwear", and "Urgent Footwear".
4. Text order: "To 2B-300 prosthetics department via wheelchair and escort for DH walker offloading boot".
Post-Operative Day #3:
Discuss/plan any foot reconstruction operation during this hospitalization or during subsequent outpatient encounter.
Along with daily aspirin, discuss continuing or initiating low-dose rivaroxaban unless: (1) already on dual antiplatelet or other anticoagulant for another indication; (2) active malignancy; (3) HAS-BLED score ≥3 or other reason to suspect high risk of bleeding; or (4) advanced liver disease or end-stage renal disease.
Consider therapeutic rivaroxaban, apixiban, or warfarin if multi-segment (spliced) vein.
Goals prior to transitioning to outpatient management: “ABC DEF”
| Letter | Action |
|---|---|
| A= | Antibiotic plan |
| B= | Blood flow follow-up (i.e. our clinic) |
| C= | Consultant follow-up (ECL wound care or Podiatry ± Infectious Disease) |
| D= | Discharge Destination: home, nursing facility, inpatient rehabilitation, other |
| E= | Equipment and supplies |
| F= | Footwear (offloading boot) and Four point walker (both from prosthetics department) |
The afternoon prior to day of anticipated transition to outpatient care:
Additional orders, day prior to transition to outpatient care:
1. Tramadol OR Tylenol #3 PO q6h as needed. Dispense 20 tablets, no refills.
2. A 30-day supply of all needed wound care supplies.
The morning of anticipated transition to outpatient care: Remove incisional wound VAC (or post-operative day #5, whichever comes first).