Healing Feet, Avoiding Amputation

GitHub page
Deep Infection? Drain/Incise
First: Be vigilant in identifying soft tissue
Foot infections are a common precursor to the decision for leg amputation. Infection can cause systemic illness (including acute kidney injury and acute coronary syndrome). Surgery is often an important component to the treatment of infection.

Foot infection should be assumed present unless proven otherwise in all patients with the following findings.
Absence of any of these findings does NOT rule infection.
| finding |
|---|
| nausea |
| anorexia |
| subjective chills or sweats |
| new onset foot pain |
| altered mental status |
| fever |
| tachycardia |
| any drainage (not only purulent) |
| foot or calf edema |
| foul odor |
| elevated white blood cell count |
| elevated serum procalcitonin |
| elevated c-reactive protein |
| acute kidney injury |
| criteria for of SIRS or septic shock |
| 2+ points on qSOFA |
Here’s a brief (5 minute 8 second) video primer on identifying foot infections:
Check out these videos if you would benefit from advice on concise patient presentations.
Admission orders
Laboratory studies
- Type and SCREEN
- CBC with differential
- Complete metabolic panel
- C-reactive protein (CRP)
- procalcitonin
- brain naturetic peptide (BNP) if new dyspnea/orthopnea, if abnormal EKG or if history of heart failure
- PT/PTT/INR only if on anticoagulation
Medications
The acronym “SAVE THe LIMB” will help you remember medications that may be important for hospitalized with foot infections:
| Letter | Medication |
|---|---|
| S= | Statin medication |
| A= | Aspirin 81mg Antibiotic: ceftriaxone 1gm IV q24h ± topical cadexomer iodine to bedside for subsequent dressing changes |
| V= | Vitamin C 500mg PO BID and Vitamin D3 25mg PO daily Vancomycin with calculated dosage only if MRSA nares swab is positive OR if pre-op. for abscess I&D. |
| E= | ”Ensure” BID (though Glucerna SR has lowest added sugar) |
| T= | Tylenol PRN for pain or temperature >100.4F |
| He= | Heparin subcutaneous q8h. Do not hold for OR. Home meds except metformin, Coumadin, other anticoagulants. |
| L= | Lactobacillus 2 caps PO BID |
| I= | Insulin: 50% of long-acting insulin home dose + sliding scale PRN |
| M= | Multivitamin 1 cap daily |
| B= | Blood pressure meds, baseline + at least one PRN for SBP>140mmHg |
Do not empirically treat for Pseudomonas, as this organism represents only 3% of isolates at our hospital. Similarly, do not empirically treat for methicillin-sensitive Staphylococcus aureus (MRSA). For those with no abscess and negative MRSA nasal swab testing is negative, MRSA has been found in foot microbiology in only 5% of our patients. This increases to 22% with either abscess or MRSA nasal swab findings and to 58% with both.
Inpatient Management: Operative Treatment of Infection
L02.435/436 (abscess lower limb, right/left ), M65.171/172 (infection) or I70.261/262 (gangrene); procedure 28003 (incision and drainage) or 28820 (toe amputation).
Objectives:
- Probe from the instigating ulcer or gangrenous area to identify abscess tracts:
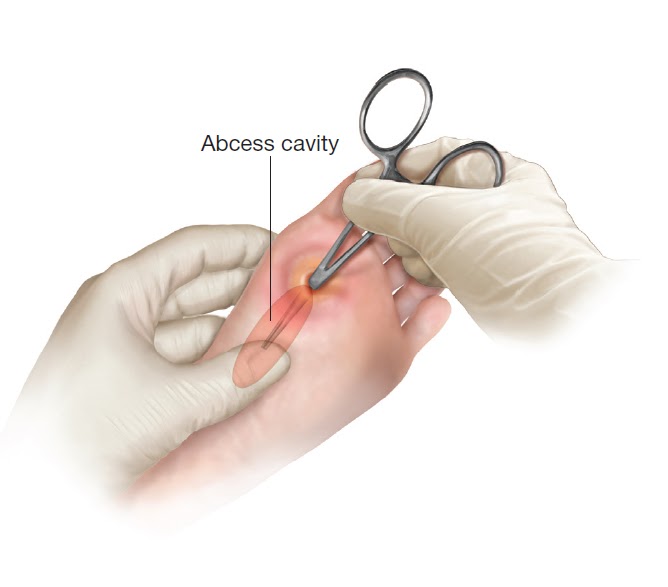
- Incision ± Penrose drain for all abscess tracts
- Collect fluid, soft tissue or bone for microbiology in sterile container with sterile saline. Swab specimens are discouraged.
- Removal of all obviously-necrotic tissue. Minimize resection of viable / marginal tissue
- Pulsatile irrigation with saline solution.
- Dress with gentamicin-impregnated 4x4 gauze in deep areas, Xeroform over shallow ulcer. Wrap with 4” inch Webril + 4” ACE from forefoot to knee to control edema.
Here is a brief (5 minute 3 second) video primer that discusses operative treatment:
Post-op orders: Continue most admission orders; saline lock IV; add diabetic diet + Glucerna BID, Iodosorb (cadexomer iodine) ointment; Do NOT order labs for POD#1
Atypical presentations:
Situation 1: hypotension (systolic blood pressure <90mmHg):
- treat like SIRS as above along with: SICU admission LR 30mL/kg (~2L) influsion over 3 hours
- intravenous vancomycin + cefipime
- norepinephrine if not responding
Situation 2: either tachycardia alone or SIRS syndrome (2+ of temperature >100.5°F or 38°C, pulse >90/minute, respiratory rate >20/minute, PaCO2<32, white blood cell count >12K/mL or 10% bands):
- get blood cultures, serum lactate, ECG, brain naturetic peptide (BNP), CK/CKMB/troponins at admission.
- Repeat EKG and BNP following day.
- Consult cardiology or vascular medicine if any are abnormal.
Situation 3: hyperosmolar hyperglycemic syndrome (HHS): serum osmolality >320 mOsm/kg. You can presume this is present if glucose >600 + sodium >140 or glucose >500 + sodium >145:
- Admit to ICU.
- Get serum ketones and q6h metabolic panels.
- Give 0.5-1L NS and start insulin drip.
- Work with medicine team to replace potassium.
Situation 4: severe hyperglycemia (glucose 300-499)
- admit to stepdown for insulin drip.
- give 500mL NS over 24 hours. .
Goals prior to transitioning to outpatient management: “ABC DEF”
| Letter | Item |
|---|---|
| A= | Antibiotic plan |
| B= | Blood flow testing |
| C= | Consultant follow-up (ECL wound care or Podiatry ± Infectious Disease) |
| D= | Discharge Destination: home, nursing facility, inpatient rehabilitation, other |
| E= | Equipment/supplies for advanced wound care |
| F= | Footwear (offloading boot) and Four point walker (both from prosthetics department) |